Patient Case Study
Case Study: Cesarean Scar Ectopic Pregnancy (CSP)
Dr. Tanuka Das Gupta
Hospital: Peerless Hospital & B K Roy Research Center
Background
Mrs. I. Ghosh, with a history of a previous cesarean section, presented with a new pregnancy. She had suffered the tragic loss of her previous child at 4 years of age.
At around 6 weeks of gestation, she experienced slight vaginal bleeding, prompting immediate medical evaluation.
Clinical Findings
An early ultrasound examination revealed a Cesarean Scar Ectopic Pregnancy (CSP)—a rare but potentially life-threatening condition.
The gestational sac was implanted over the previous uterine scar, protruding towards the abdominal cavity instead of growing within the uterine cavity.
Risk Assessment
Cesarean scar ectopic pregnancy carries serious risks, including:
Uterine rupture
Massive hemorrhage
Emergency hysterectomy
Compromised future fertility
The primary objective in this case was to save the uterus and prevent life-threatening complications.
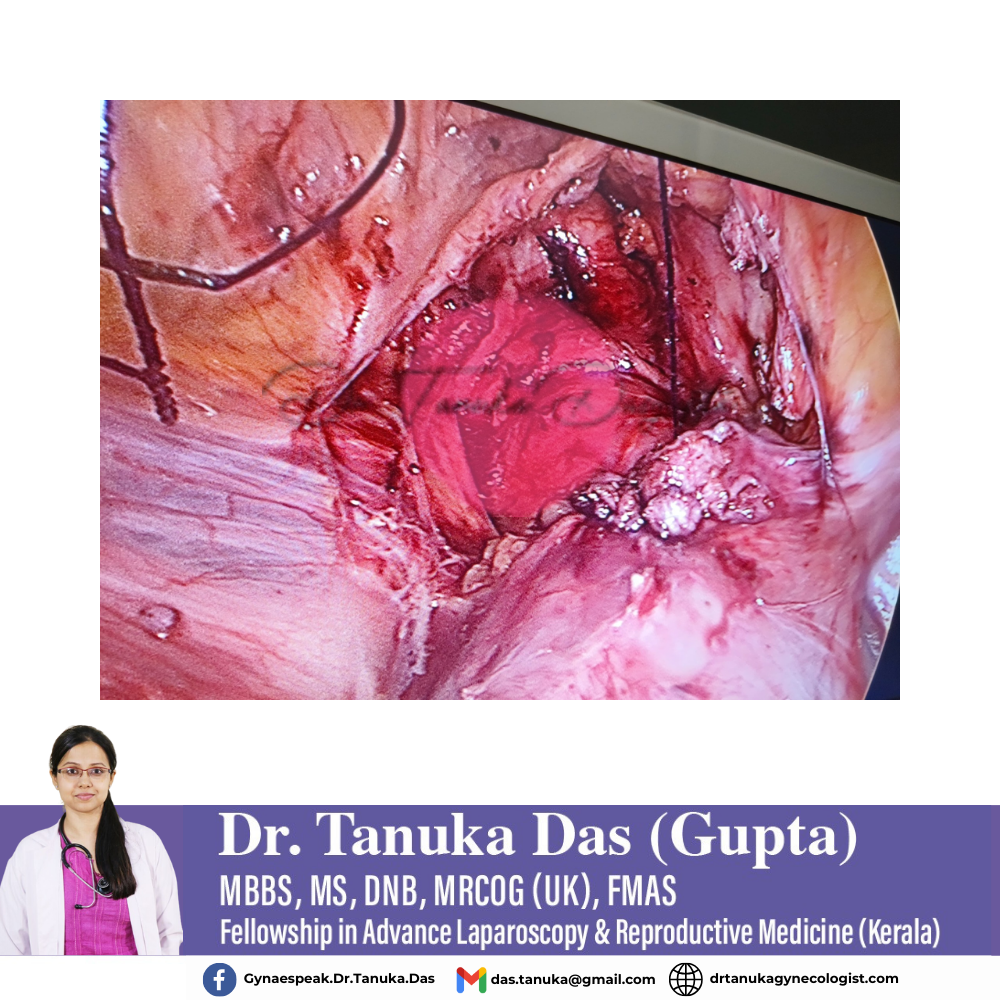
Management & Treatment
Under the care of Dr. Tanuka Das Gupta, a laparoscopic removal of the scar ectopic pregnancy was performed, followed by meticulous repair of the uterine scar.
The procedure was conducted successfully with:
No significant blood loss
No intraoperative complications
Outcome
The patient had an uneventful recovery
Discharged the very next day
Uterus successfully preserved
Advised regular follow-up and future pregnancy planning under close supervision
Clinical Insight
Cesarean Scar Ectopic Pregnancy (CSP) is rare but extremely serious.
Early diagnosis through timely ultrasound and expert surgical management can be life-saving and fertility-preserving.
Key Message:
Awareness, early detection, and minimally invasive surgery can prevent catastrophic outcomes in cesarean scar ectopic pregnancies.
#CesareanScarEctopic #CSP #HighRiskPregnancy #LaparoscopicSurgery #UterusPreservation #DrTanukaDasGupta

Case Study: Life-Threatening Hemoperitoneum in a Patient with Glanzmann Thrombasthenia
Patient Profile
A 19-year-old young woman with a rare negative blood group and a known platelet function disorder—Glanzmann thrombasthenia presented in a critical condition.
Presentation
She was admitted with:
Severe abdominal pain
Massive internal bleeding (hemoperitoneum)
Hemoglobin level of only 4 g/dL, indicating life-threatening blood loss
Imaging revealed blood collected inside the abdomen, secondary to a spontaneous rupture of an ovarian cyst, precipitated by her underlying platelet dysfunction.
Clinical Challenge
This case demanded a highly coordinated, multidisciplinary approach due to:
Extremely low hemoglobin
Rare negative blood group, making blood procurement difficult
Severe platelet functional defect causing uncontrolled bleeding
The patient’s father was extremely supportive, which played a crucial role in timely decision-making and care.
Multidisciplinary Management
Successful management required close collaboration between:
Hematologist – for managing Glanzmann thrombasthenia and transfusion strategy
Intensivist – for hemodynamic stabilization and critical care
Surgical team – for definitive management of intra-abdominal bleeding
Arranging compatible negative blood group transfusions was challenging but achieved through coordinated efforts.
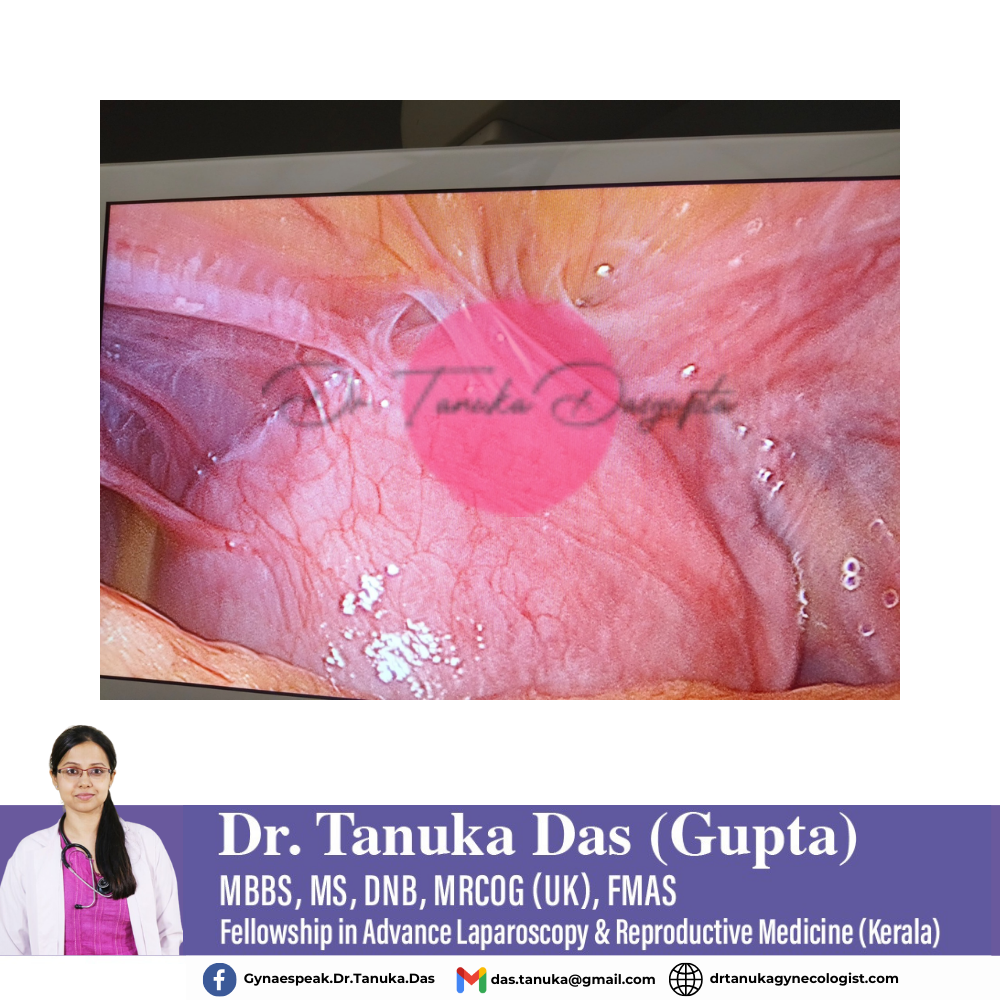
Surgical Intervention
A laparoscopic procedure was performed to:
Evacuate approximately 750 ml of blood from the abdominal cavity
Control bleeding following rupture of the ovarian cyst
Minimize surgical trauma and blood loss in a high-risk patient
Despite the complexity, the procedure was completed successfully.
Outcome
The patient stabilized well post-operatively
No further bleeding episodes
Gradual improvement in hemoglobin levels
Discharged in stable condition
She is currently doing well, with continued follow-up advised.
Conclusion
This case highlights the critical importance of a well-equipped multi-specialty hospital, early surgical intervention, and seamless teamwork in managing rare hematological disorders with acute gynecological emergencies.
Wishing this brave young woman a lifetime of happiness, strength, and good health.


